Post-operative Sensitivity: Causes, Prevention & Management
- Dr. Divij Khullar

- Dec 22, 2025
- 2 min read

Post-operative sensitivity is one of the most common complaints after restorative procedures, scaling, crown preparation, and even endodontic therapy. While most cases are mild and temporary, unmanaged sensitivity can lead to patient discomfort and reduced trust in treatment outcomes. Students enrolled in dental courses in Delhi NCR, or pursuing advanced clinical training, must understand how to prevent, diagnose, and manage post-operative sensitivity effectively.
What Is Post-operative Sensitivity?
Post-operative sensitivity refers to transient pain or discomfort triggered by cold, heat, air, or chewing after a dental procedure. It typically arises from exposed dentinal tubules or irritation to pulp tissue.
Common symptoms include:
Sharp pain on biting
Sensitivity to cold air or fluids
Short, sharp discomfort
Tenderness during chewing
Causes of Post-operative Sensitivity
Dental interns should be aware of the main clinical factors that contribute to sensitivity:
1. Dentinal Exposure
Occurs after cavity preparation, scaling, or crown reduction. Open tubules transmit stimuli to the pulp, causing discomfort.
2. Polymerisation Shrinkage in Composites
Incorrect layering or curing techniques may create micro-gaps, leading to leakage and sensitivity.
3. High Occlusal Contacts
Premature contacts after restorative procedures can aggravate periodontal ligaments, causing pain.
4. Overheating During Tooth Preparation
Insufficient coolant during rotary instrumentation may irritate the pulp.
5. Gingival Retraction Trauma
Improper cord placement can cause localised inflammation and discomfort.
6. Endodontic Irritation
Irrigant extrusion, over-instrumentation or missed canals may trigger post-operative pain.
How to Prevent Post-operative Sensitivity
Preventive strategies ensure smoother treatment outcomes and improved patient satisfaction.
1. Use Conservative Preparation Techniques
Preserve enamel when possible - enamel provides better bonding and less sensitivity.
2. Follow Proper Composite Layering Protocols
use incremental placement
minimise polymerisation shrinkage
ensure adequate curing
3. Maintain Ideal Occlusion
Always check occlusion in both centric and excursive movements before dismissing the patient.
4. Ensure Proper Cooling During Tooth Preparation
Adequate water spray prevents pulpal irritation.
5. Use Desensitising Agents
Dentin bonding agents and varnishes can seal tubules effectively.
Management of Post-operative Sensitivity
Most cases resolve on their own, but active management reassures patients and prevents complications.
1. Adjust Occlusion
High points should be corrected immediately.
2. Recommend Desensitising Toothpaste
Potassium nitrate or arginine-based pastes reduce discomfort.
3. Apply Fluoride Varnish
Strengthens enamel and seals dentinal tubules.
4. Reevaluate Restorations for Microleakage
Leaking composite margins may require refurbishment or replacement.
5. Provide Clear Post-treatment Instructions
Avoid extreme temperature foods for 24-48 hours. Inform patients that mild sensitivity is normal.
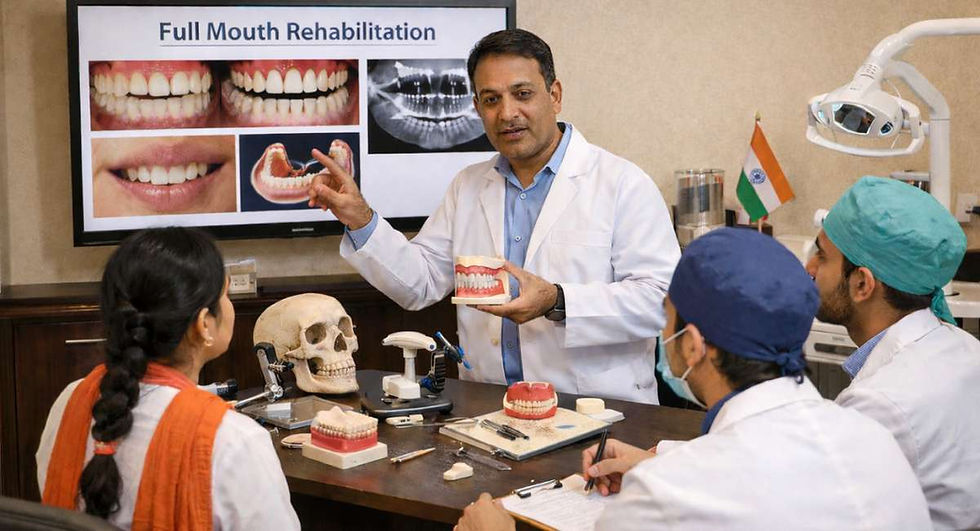
The Role of Training & Mentorship
At Dr Khullar’s Dental Academy, interns are taught evidence-based restorative techniques that reduce post-operative complications. Students in dental courses in Delhi NCR benefit from hands-on training that refines their clinical judgment and technique precision.
Conclusion
Post-operative sensitivity is predictable and preventable when clinicians follow proper protocols. With strong foundational training and attention to detail, dental interns can confidently manage patient expectations and deliver long-term, comfortable restorations. Training at a reputable Dental Academy in Delhi NCR ensures that students develop these essential skills early in their careers.




Comments